Four Visions of the Future of US IVF
Network and Do-It-Yourself, Academic and Allocator
Some of my favorite virtual IVF think-tankers, Steve Rooks, Dr. Steven Young, Dr. Eve Feinberg (and I think I see Dr. Paula Amato lurking somewhere in the background) engaged in a LinkedIn debate over the holiday weekend regarding the role of academic centers in the present and future of IVF.
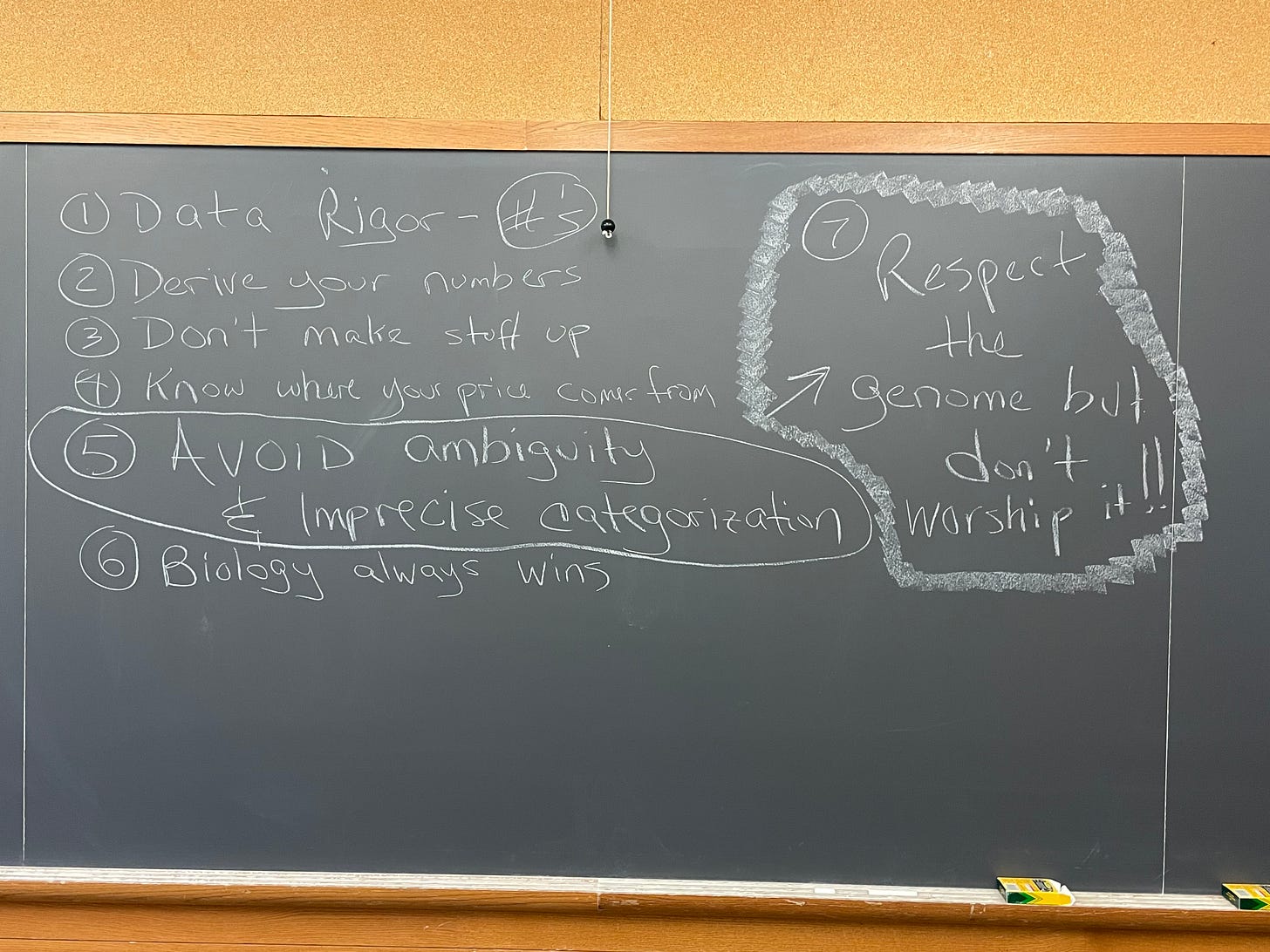
(Hamilton Hall, Columbia University — Entrepreneurship in Biotechnology week 10)
I've given some thought to the topic, and I think that academic IVF is too easily (and unfairly) dismissed. It is filled with extremely talented individuals (look no further than Drs. Young and Feinberg) and uniquely capable of taking advantage of a rapidly evolving ecosystem and addressing a chronically underserved (but actually quite large and important) constituency.
A brief digression: unique among medical subspecialties, infertility, and assisted reproduction are blessed (or cursed, depending on your track record) with one of the few unequivocal endpoints in all of epidemiology: live birth per euploid embryo transferred.
One of the benefits of spending half my professional life in biotechnology is the development over two decades (a smarter person than me would have needed a lot less time) of a sixth sense for good data. Step one is identifying good data -- the type that lets you truthfully answer clinically relevant questions and solve patients' problems faster, cheaper, and in a more painless and convenient way.
And good data means a good endpoint. A measurement that matters.
IVF pregnancy rates, with certain limitations for patient mix, are among the most unequivocal endpoints in clinical medicine. IVF outcomes have no moral victories: it's baby or not. Sum up all of your embryo transfers and show us the data.
No visual analog scores on the wall of the hospital room with the happy "no pain" faces on one side and the suffering red "real bad pain" on the other.
This reliance on unequivocal data gives lesser-known names in the IVF world the ability to develop differently engineered delivery systems that take a patient from "I need help to have a baby" to having a baby, at lower out-of-pocket cost, faster throughput from self-identification to outcome, and potentially less disruption to the rest of life.
A few years back, I posted a piece on the Do-It-Yourself IVF cycle, one coordinated by the patients themselves, stitching together the various components of an IVF cycle from a combination of online, local distance resources accessed in-person or remotely.
I temporarily lost a few friends in the field (they all came back) with my suggestion that a patient, acting as their own travel agent, could successfully navigate an IVF ecosystem that included independent diagnostics, separated stimulation, retrieval, and vitrification from the rest of embryology and embryo transfer, and had either improved market transparency or an easily accessed care coordination industry separate from the large IVF networks.
I still think that DIY IVF is one of the paths to a million IVF babies a month, but there are other equally valid and viable paths.
One is my idealized virtual Bell Labs of IVF (cue my close friends and colleagues to roll their eyes now, having heard this so many times)—a system where we get a bunch of talented IVF doctors, scientists, nurses, and genetics people together with an equally talented team of systems engineers and data masters and engineer the hell out of the IVF process, from patient realization that they need help to discharge to obstetrical care.
Is the Virtual Bell Labs of IVF a real possibility? Sure. In theory, it could come from inside one of the dominant IVF networks, one that wants to tap into the larger, untreated population of people with infertility, habitual pregnancy loss, genetic disease risk or accelerated infertility due to lifesaving but sterilizing cancer treatment who lack either financial, geographic or "ain't possible to dedicate that much time to an IVF cycle" ability to enter the current marketplace.
More so than other areas of medicine and healthcare, consolidation and expansion of the best-performing IVF networks in the United States has been a patient-positive development, leading to more rapid adoption of best practices, decreases in the dollars-to-baby cost of the procedure, and transparent improvements in quality of care. But --
But these networks, often funded and backed by private equity (there is nothing wrong with private equity funding -- it's just one more source of expansion capital, and there are good and bad private equity agreements) do not possess the organizational DNA that incentivizes super-incremental innovation. Many (but not all) PE firms have too short a time horizon for exiting their investments to allocate more than a token amount to the development of a totally separate and parallel system of care, even if that system could ultimately overtake the incumbent system in terms of size and economic opportunity.
So, who could? Maybe academic medical centers with interdisciplinary access to superb engineering talent and process optimization expertise, a desire (and professional incentive) to experiment and scale change, and a mandate to expand and improve care.
Or maybe an emerging allocator class, a concept that morphs the "Do-It-Yourself IVF Cycle" concept into a "Let Us Help You Do-It-Yourself" system.
The allocator system may grow out of or be part of our post-2016 employer-based IVF coverage administration world, or it may be the next, more sophisticated version of the cycle buyer/bundlers that we have seen in the past, taking advantage of technology that disaggregates cycles from the central big box laboratory model into more modular options which may be cheaper, closer to home, more compatible with the realities of normal life during the IVF cycle -- yet still validated by the best data endpoint in healthcare.
Or maybe the allocator class will emerge from academia, leveraging science, data, business, and systems expertise to rewrite IVF care for rare disease clinics, cancer centers, and centers of excellence that don't exist anywhere else.
Don’t discount academic IVF centers.
More to come.


I'm all in on the virtual Bell Labs of IVF approach David!